High-Quality Colon Cancer Treatment Cost In India
How Much Does Colon Cancer Treatment Cost In India?
“The average cost of colon cancer treatment in India starts from $5,000. In some cases, it may reach as high as $15,500 depending on hospital location and doctor experience. However, this cost is still far less than what it costs in other countries.”

Overview
Colon cancer is a cancer that starts in the colon (large intestine) or rectum. Both of these organs are in the lower portion of your digestive system. The rectum is at the end of the colon.
Most of the time colon cancer affects adults, though it can happen at any age. It usually begins as small tumor in large intestine, noncancerous (benign) group of cells called tumor that form on the inside of the colon. Over time some of these tumor can become colon cancers.
Tumor may be small and produce few, if any, symptoms. For this reason, doctors recommend regular screening tests to help control colon cancer by identifying and removing tumor before they turn into cancer.
If colon cancer develops, many treatments are available to help control it, including surgery, radiation therapy and drug treatments, such as chemotherapy, targeted therapy and immunotherapy.
Colon cancer is also called as colorectal cancer, which is a term that combines colon cancer and rectal cancer, which begins in the rectum.
Signs and symptoms of colon cancer
- A determined change in your bowel habits, including diarrhea or constipation or a change in the consistency of your stool
- Rectal bleeding or blood in your stool
- abdominal pain, cramping, bloating, or gas
- A feeling that your bowel doesn’t empty completely
- continual urges to defecate despite passing stools
- Weakness or fatigue
- Unexplained weight loss
- irritable bowel syndrome
Many people with colon cancer experience no symptoms in the early stages of the disease. When symptoms appear, they’ll likely vary, depending on the cancer’s size and location in your large intestine.
Risk of Colon Cancer
Factors that may increase your risk of colon cancer include:
- Older age. Colon cancer can be diagnosed at any age, but a Most of people with colon cancer are older than 50 years old.
- A personal history of colorectal cancer or polyps. If you’ve already had colon cancer or noncancerous colon polyps, More risk in future of colon cancer.
- Inflammatory intestinal conditions. Chronic inflammatory diseases of the colon, such as ulcerative colitis and Crohn’s disease, can increase your risk of colon cancer.
- Inherited syndromes that increase colon cancer risk. Some gene mutations passed through generations of your family can increase your risk of colon cancer significantly. Only a small percentage of colon cancers are linked to inherited genes. The most common inherited syndromes that increase colon cancer risk are familial adenomatous polyposis (FAP) and Lynch syndrome, which is also known as hereditary nonpolyposis colorectal cancer (HNPCC).
- Family history of colon cancer. You’re more likely to develop colon cancer if you have a blood relative who had colon cancer before. If more than one family members had affected with colon cancer or rectal cancer, your risk is even greater.
- Low-fiber, high-fat diet. Colon cancer and rectal cancer may be associated with a typical Western diet, which is low in fiber and high in fat and calories. Research in this area has had mixed results. Some studies have found an increased risk of colon cancer in people who eat diets high in red meat and processed meat.
- A sedentary lifestyle. People who are not active are more likely to develop colon cancer. doing regular physical activity may reduce your risk of colon cancer.
- Diabetes. People with diabetes or insulin resistance have an increased risk of colon cancer.
- Obesity. People who are obese have an increased risk of colon cancer and an increased risk of dying of colon cancer when compared with people considered normal weight.
- Smoking. People who smoke may have an increased risk of colon cancer.
- Alcohol. Heavy use of alcohol increases your risk of colon cancer.
- Radiation therapy for cancer. Radiation therapy directed at the abdomen to treat previous cancers increases the risk of colon cancer.
Lifestyle that reduce your risk of colon cancer
Here is some of the step to reduce risk of colon cancer through changes in your day to day life
- Eat a variety of fruits, vegetables and whole grains. Fruits, vegetables and whole grains contain vitamins, minerals, fiber and antioxidants, which may play a role in cancer prevention. Choose a variety of fruits and vegetables so that you get an array of vitamins and nutrients.
- Stop smoking. there is many way to stop smoking . talk to your doctor about ways to quit that may work for you.
- Drink alcohol in moderation, if at all. If you want to drink alcohol, drink in limit. don’t drink more than one drink a day for women and two for men.
- Exercise most days of the week. Try to get at least 30 minutes of exercise on most days. If you’ve been inactive, start slowly and build up gradually to 30 minutes. Also, talk to your doctor before starting any exercise program.
How is Colon cancer diagnosed?
Doctors use many tests to find or diagnose, cancer. They also do tests to learn if cancer has spread to another part of the body from where it started. If this happens, it is called metastasis. For example, imaging tests can show if cancer has spread. Imaging tests show pictures of the inside of the body. Doctors may also do tests to learn which treatments could work best.
- Colonoscopy. As described in Screening, a colonoscopy allows the doctor to look inside the entire rectum and colon while a patient is sedated. A colonoscopist is a doctor who specializes in performing this test. If colon cancer is found, a complete diagnosis that accurately describes the location and spread of the cancer may not be possible until the tumor is surgically removed.
- Biopsy. Taking small amount of tissue from the tumor for examination under a microscope. Other tests can suggest that cancer is present, but only a biopsy can make sure the diagnosis of colon cancer. A pathologist then analyzes the sample(s). A pathologist is a doctor who specializes in interpreting laboratory tests and evaluating cells, tissues, and organs to diagnose disease. A biopsy may be performed during a colonoscopy, or it may be done on any tissue that is removed during surgery.
- Biomarker testing of the tumor. Biomarker testing is a way to look for genes, proteins, and other substances (called biomarkers or tumor markers) that can provide information about cancer. Each person’s cancer has a unique pattern of biomarkers. Some biomarkers affect how certain cancer treatments work. Biomarker testing may help you and your doctor choose the best treatment for you.
- Blood tests. Because colorectal cancer often bleeds into the large intestine or rectum, people with the disease may become anemic. A test of the number of red cells in the blood, which is part of a complete blood count (CBC), can indicate that bleeding may be occurring.
Another blood test detects the levels of a protein called carcinoembryonic antigen (CEA). High levels of CEA may indicate that a cancer has spread to other parts of the body. CEA is not a perfect test for colorectal cancer because levels are high for only about 60% of people with colorectal cancer that has spread to other organs from the colon. In addition, other medical conditions can cause CEA to increase. A CEA test is most often used to monitor colorectal cancer for people who are already receiving treatment. It is not useful as a screening test. Learn more about tumor markers for cancer.
- Computed tomography (CT or CAT) scan. A CT scan takes pictures of the inside of the body using x-rays taken from different angles. A computer combines these pictures into a detailed, 3-dimensional image that shows any abnormalities or tumors. A CT scan can be used to measure the tumor’s size. Sometimes a special dye called a contrast medium is given before the scan to provide better detail on the image. This dye can be injected into a patient’s vein or given as a pill or liquid to swallow. In a person with colon cancer, a CT scan can check for the spread of cancer to the lungs, liver, and other organs. It is often done before surgery (see Types of Treatment).
- Magnetic resonance imaging (MRI). An MRI uses magnetic fields, not x-rays, to produce detailed images of the body. MRI can be used to measure the tumor’s size. A special dye called a contrast medium is given before the scan to create a clearer picture. This dye can be injected into a patient’s vein or given as a pill or liquid to swallow. MRI is the best imaging test to find where the colorectal cancer has grown.
- Ultrasound. An ultrasound uses sound waves to create a picture of the internal organs to find out if cancer has spread. Endorectal ultrasound is commonly used to find out how deeply rectal cancer has grown and can be used to help plan treatment. However, this test cannot accurately detect cancer that has spread to nearby lymph nodes or beyond the pelvis. Ultrasound can also be used to view the liver, although CT scans or MRIs (see above) are better for finding tumors in the liver.
- Chest x-ray. An x-ray is a way to create a picture of the structures inside of the body, using a small amount of radiation. An x-ray of the chest can help doctors find out if the cancer has spread to the lungs.
- Positron emission tomography (PET) or PET-CT scan. A PET scan is usually combined with a CT scan (see above), called a PET-CT scan. However, you may hear your doctor refer to this procedure just as a PET scan. A PET scan is a way to create pictures of organs and tissues inside the body. A small amount of a radioactive sugar substance is injected into the patient’s body. This sugar substance is taken up by cells that use the most energy. Because cancer tends to use energy actively, it absorbs more of the radioactive substance. However, the amount of radiation in the substance is too low to be harmful. A scanner then detects this substance to produce images of the inside of the body. PET scans are not regularly used for all people with colorectal cancer, but there are specific situations when your doctor may recommend one.
Colon Cancer Stages
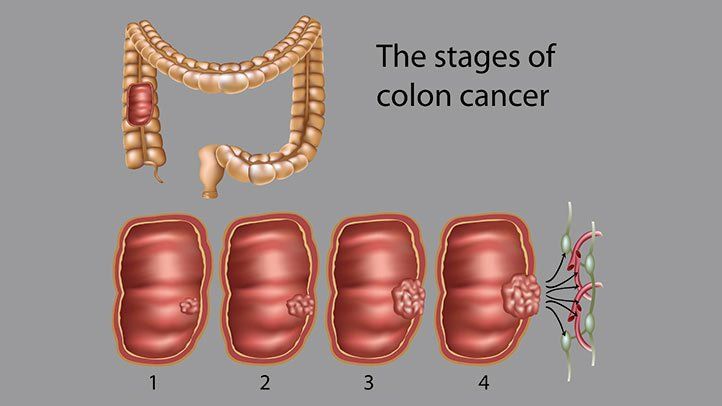
- Stage 0. Also known as carcinoma in situ, in this stage abnormal cells are only in the inner lining of the colon or rectum.
- Stage 1. The cancer has penetrated the lining, or mucosa, of the colon or rectum and may have grown into the muscle layer. It hasn’t spread to nearby lymph nodes or to other parts of the body.
- Stage 2. The cancer has spread to the walls of the colon or rectum or through the walls to nearby tissues but hasn’t affected the lymph nodes.
- Stage 3. The cancer has moved to the lymph nodes but not to other parts of the body.
- Stage 4. The cancer has spread to other distant organs, such as the liver or lungs.
Type of Colon Cancer Treatment

Which treatments are most likely to help you depends on your particular situation, including the location of your cancer, its stage and your other health concerns. Treatment for colon cancer usually involves surgery to remove the cancer. Other treatments, such as radiation therapy and chemotherapy, might also be recommended.
Surgery
- Removing polyps during a colonoscopy (polypectomy). If your cancer is small, localized, completely contained within a polyp and in a very early stage, your doctor may be able to remove it completely during a colonoscopy.
- Endoscopic mucosal resection. Larger polyps might be removed during colonoscopy using special tools to remove the polyp and a small amount of the inner lining of the colon in a procedure called an endoscopic mucosal resection.
- Minimally invasive surgery (laparoscopic surgery). Polyps that can’t be removed during a colonoscopy may be removed using laparoscopic surgery. In this procedure, your surgeon performs the operation through several small incisions in your abdominal wall, inserting instruments with attached cameras that display your colon on a video monitor. The surgeon may also take samples from lymph nodes in the area where the cancer is located.
- Partial colectomy. During this procedure, the surgeon removes the part of your colon that contains the cancer, along with a margin of normal tissue on either side of the cancer. Your surgeon is often able to reconnect the healthy portions of your colon or rectum. This procedure can commonly be done by a minimally invasive approach (laparoscopy).
- Surgery to create a way for waste to leave your body. When it’s not possible to reconnect the healthy portions of your colon or rectum, you may need an ostomy. This involves creating an opening in the wall of your abdomen from a portion of the remaining bowel for the elimination of stool into a bag that fits securely over the opening.
Sometimes the ostomy is only temporary, allowing your colon or rectum time to heal after surgery. In some cases, however, the colostomy may be permanent. - Lymph node removal. Nearby lymph nodes are usually also removed during colon cancer surgery and tested for cancer.
Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells. For people with colorectal cancer, chemotherapy commonly takes place after surgery, when it’s used to destroy any lingering cancerous cells. Chemotherapy also controls the growth of tumors.
Radiation Therapy
Radiation Therapy uses a powerful beam of energy, similar to that used in X-rays, to target and destroy cancerous cells before and after surgery. Radiation therapy commonly occurs alongside chemotherapy.
Immunotherapy
This aims to increase the immunity of the body to help attack and destroy the cancer cells. Drugs are administered to increase the immunity of the body through oral or intravenous routes.
Targeted therapy
This treatment uses medicines that specifically target the cancer cells without causing any great damage to healthy cells. The medicines target cell components that are involved in cancer cell division.
Before the procedure
- Your doctor will explain the surgical procedure to you. Ask any questions that you might have about the procedure. Be sure you understand what the extent of the surgery is likely to be and what you should expect afterward.
- You may be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully and ask questions if something is not clear.
- Ask your doctor if you will possibly need a blood transfusion. If the doctors think a transfusion might be needed, you might be asked to donate blood beforehand.
- Your doctor will go through your full medical history and additionally may perform a complete physical examination to ensure you are in good health before undergoing the procedure. You may undergo blood tests or other diagnostic tests.
During the procedure
Surgery is the removal of the tumor and surrounding tissue during an operation. Procedures may vary depending on your condition and your doctor’s practices.
Generally, the surgery follows this process:
- You will be asked to remove clothing and put on a hospital gown.
- An intravenous (IV) line may be started in your arm or hand.
- You will be positioned on the operating table.
- A urinary catheter may be inserted.
- The surgery will be performed while you are asleep under general anesthesia. The anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the surgery.
- Depending on the stage of your cancer and overall medical condition, the surgeon
After the procedure
In the hospital
The patient requires a stay in the hospital for 5-7 days depends on the patient’s condition and complication. After the surgery, you will be taken to the recovery room for observation. The staff will monitor your blood pressure, pulse, alertness, pain or comfort level, and your need for medications and give you medicine for pain. When they are sure that you are stable, you will be transferred to a room in the hospital.
Follow-up Care
It is vial post-treatment for colorectal cancer. Your doctors monitor recovery and check for the recurrence of cancer. Get a schedule for follow-up exams and tests post-treatment. Also, get suggestions for diet and physical activity post-treatment. Watch out for long-term side effects from your treatment and contact your doctor. Get Low-Cost Colorectal Treatment in India by contacting us.
Frequently Asked Questions About Colon Cancer
Q. Can colon cancer be cured?
Q. Cancer of the colon is a highly treatable and often curable disease when localized to the bowel. Surgery is the primary form of treatment and results in cure in approximately 50% of the patients. Recurrence following surgery is a major problem and is often the ultimate cause of death.
Q. Can you live a normal life after colon cancer?
A. The Most of patients diagnosed with colon cancer can be treated and will go on to live normal lives.
