Fontan Procedure Cost in India
How Much Does Fontan Procedure Cost In India?
The Fontan Procedure in India is substantially less expensive than in other countries, making it more accessible to patients. However, the Fontan Procedure Cost in India starts from USD 5,000 to USD 9,000. Furthermore, India is home to some of the Best Cardiac Surgeon in India who have extensive training and expertise in carrying out the Fontan Procedure.
- 10-14 days stay in the hospital including ICU admission.
- Duration of 4-7 hours of surgery
- 25-30 days of stay in the country
- Doctor’s team consultation fees
- Surgical costing
- Pre and Post operative care and all medical Tests
Overview
The Fontan Procedure is a surgical procedure used for treating cardiac conditions such tricuspid atresia and hypoplastic left heart syndrome. During this treatment, the doctor modifies the cardiac structure so that certain regions of the heart can be bypassed and blood can flow more effectively to the lungs.
During Fontan Procedure in India, a surgery is carried out to treat Hypoplastic Left Heart Syndrome, a congenital defect in which a newborn has only one functional ventricle. In this syndrome, oxygen-rich and oxygen-depleted blood are mixed in the circulation, turning a child blue. After two other procedures, the Fontan procedure is performed when a child is between the ages of 18 months and two years.
What Is a Fontan Procedure ?
A Fontan Procedure in India improves circulation in individuals who only have one functional ventricle in their heart. This condition occurs as a result of one of several congenital heart disorders.
This surgical intervention, known as the Fontan surgery, enables blood low in oxygen from the lower body to bypass the heart and directly reach the pulmonary artery, facilitating oxygenation in the lungs. Typically, this procedure follows a preceding operation, the Glenn procedure, which redirects oxygen-depleted blood from the upper body to the pulmonary artery and lungs.
Subsequent to undergoing the Fontan Procedure in India, all oxygen-depleted blood is channeled exclusively through the pulmonary artery to the lungs, eliminating the need for its passage through the heart. This blood flow occurs passively, without reliance on a pumping ventricle.
The heart is comprised of four chambers:
- Two upper chambers called atria
- Two lower chambers known as ventricles
When one of these ventricles or a principal heart valve fails to develop properly before birth, the other ventricle assumes the role of compensating for the underdeveloped or non-functional ventricle.
Right Candidate for Fontan Procedure?
Children between the ages of 2 and 15 (typically 3 to 5) who were born with a single ventricle condition will be a Right Candidate for Fontan heart Procedure in India. However, it is not for everyone. The doctor treating your child will determine whether or not they are a good candidate for the Fontan procedure. For example, their functional ventricle must be powerful enough to pump effectively, and their lungs must be in good enough condition to receive passive blood flow.
Before receiving a Fontan heart treatment, your child will likely need to undergo at least one prior procedure, such as:
- Norwood Procedure
- Glenn Procedure
- Blalock-Taussig-Thomas (BTT) shunt
- Pulmonary Artery Band
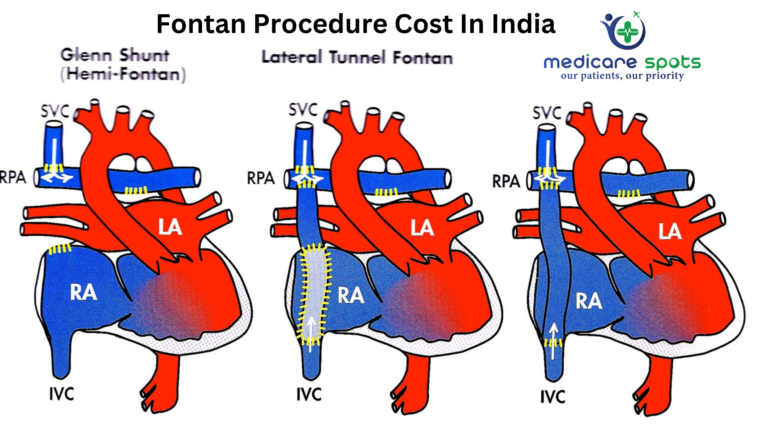
How Many Types of Fontan Procedures?
Fontan procedures in India can be performed in a variety of methods. The Types of Fontan Procedure in India are defined mostly by the specific kind of cardiac defect. The three ways listed below will help to restore blood flow:
Classic Fontan Procedure: This is the original Fontan procedure that redirects oxygen-depleted blood from the lower body directly to the pulmonary artery. It involves creating a connection between the inferior vena cava (IVC) and the pulmonary artery, allowing blood to flow to the lungs for oxygenation.
Atriopulmonary Connection (APC) Fontan: In this variation, the connection between the inferior vena cava (IVC) and the pulmonary artery is made using the atrial wall. This approach can be used when the size or anatomy of the IVC is not conducive to a direct connection.
Total Cavopulmonary Connection (TCPC) Fontan: This approach involves connecting both the superior and inferior vena cavae directly to the pulmonary arteries. The TCPC Fontan is further divided into different types based on the specific connections made, such as lateral tunnel and extracardiac conduit.
Hemi-Fontan Procedure: This is an intermediate stage between the Glenn procedure and the Fontan completion. It involves connecting the superior vena cava (SVC) directly to the pulmonary arteries, while the IVC continues to deliver blood to the heart. The Fontan completion is performed at a later stage.
Bicaval Fontan: This procedure involves connecting both the superior and inferior vena cavae to the pulmonary arteries without using an intra-atrial baffle. This approach aims to improve the efficiency of blood flow.
Fenestrated Fontan: In some cases, a small hole (fenestration) is intentionally left in the Fontan circulation to allow a controlled amount of blood to flow back into the heart. This can help relieve pressure and reduce complications, especially in the early post-operative period. The fenestration may be closed later if the patient’s condition improves.
It’s important to note that the choice of Fontan procedure depends on factors such as the patient’s individual anatomy, overall health, and specific heart defect. Cardiac surgeons and medical teams will evaluate each patient’s case to determine the most suitable approach.
Before the Procedure?
After your child’s healthcare professional determines that he or she is a candidate for the Fontan procedure, they will do testing that may include:
- Transthoracic echocardiogram (TTE).
- Electrocardiogram (EKG).
- Heart catheterization.
- Pulmonary assessment (checking your child’s breathing and oxygen level).
- Imaging, such as CT or MRI, in some cases.
During Fontan Procedure?
The Fontan procedure is a complex surgical intervention that involves redirecting blood flow in individuals with congenital heart defects that leave them with only one functional ventricle. During the Fontan procedure, several key steps are taken to achieve the desired redirection of blood flow. Keep in mind that the specific details of the procedure may vary based on the patient’s unique anatomy and the surgical approach chosen by the medical team. Here is a general overview of what happens during the Fontan procedure:
Anesthesia: The patient is given anesthesia to ensure that they are unconscious and pain-free during the surgery. Anesthesia also helps to keep the patient’s vital signs stable throughout the procedure.
Incision: A surgical incision is made in the chest to access the heart. The specific location and size of the incision may vary based on the surgical approach chosen by the medical team.
Cardiopulmonary Bypass (CPB): In many cases, the Fontan procedure is performed using a heart-lung machine (cardiopulmonary bypass). The heart-lung machine temporarily takes over the functions of the heart and lungs, allowing the surgical team to work on the heart while keeping blood circulating and oxygenated.
Connection of Blood Vessels: The main objective of the Fontan procedure is to redirect oxygen-depleted blood from the body directly to the pulmonary arteries without passing through the non-functional ventricle. The specific connections made during the procedure may vary depending on the patient’s anatomy and the chosen surgical technique (e.g., Classic Fontan, Total Cavopulmonary Connection, etc.).
- Inferior Vena Cava (IVC) Connection: The inferior vena cava, which carries oxygen-poor blood from the lower body, is typically connected to the pulmonary artery or its branches. This allows blood to flow directly to the lungs for oxygenation.
- Superior Vena Cava (SVC) Connection: In some cases, the superior vena cava, which carries oxygen-poor blood from the upper body, may also be connected to the pulmonary artery.
Closure and Testing: Once the connections are made, the surgical team carefully tests the new circulation to ensure that blood flow is functioning properly and that there are no leaks or obstructions.
Weaning Off Bypass: After confirming the success of the procedure, the patient is gradually weaned off the heart-lung machine and the heart is allowed to resume its normal pumping function.
Closure of Incision: The surgical incision is closed using sutures or other closure techniques.
Recovery: The patient is transferred to the intensive care unit (ICU) for close monitoring during the initial stages of recovery. Over the next several days or weeks, the medical team will closely monitor the patient’s progress, manage pain, and address any potential complications.
It’s important to note that the Fontan procedure is a highly specialized surgery that requires a skilled and experienced surgical team. The specific steps and techniques used during the procedure can vary based on the patient’s individual needs and the medical center’s expertise. Additionally, advances in medical technology and surgical techniques may lead to variations in the procedure. Always consult with a medical professional for the most accurate and up-to-date information.
Risks Associated with Fontan Procedure?
- The stenosis (narrowing) of the pulmonary arteries causes pulmonary hypertension (increased pulmonary blood pressure).
- Due to atrioventricular valve regurgitation, blood can backflow from the atrium into the ventricle.
- The surgically placed duct or tube has stenosis (narrowing).
- Formation of blood clots and emboli, especially pulmonary embolism.
- Increased pressure in the IVC causes liver damage (cirrhosis), liver failure, liver cancer, and elevated blood pressure in the liver blood arteries (portal hypertension).
- Ischemia, infarction, and the inability to participate in strenuous exercise are all symptoms of ventricular failure.
- Pleural effusion, a buildup of fluid surrounding the lungs, causes breathlessness and a prolonged hospital stay.
- Intolerance to exercise
- There could be liver problems, such as hepatic fibrosis.
- Patients may require a heart transplant after a few years.
The Most Important Frequently Asked Questions
Q: What are the three Fontan stages?
A. Fontan palliation for tricuspid atresia is comprised of three sequential stages:
(a) The initial stage entails the placement of an artificial shunt connecting the right subclavian artery and the right pulmonary artery.
(b) The second stage involves creating an anastomosis between the right pulmonary artery and the superior vena cava.
(c) The third stage involves the completion of the Fontan circulation.
Q: What’s the difference between Glenn and Fontan?
A: The Glenn procedure acts as a bridge connecting the Norwood and Fontan surgeries. Within the comprehensive single ventricle surgical strategy, it holds significance by priming the heart and lungs for the passive lung circulation characteristic of the third surgery, the Fontan procedure.
Q: What are the risks of the Fontan procedure?
A: Contraindications ,Hypoplasia of the pulmonary arteries, Significant mitral regurgitation and left ventricular dysfunction ,A high level of pulmonary vascular resistance.
Q: What happens after Fontan?
A: Fontan-related morbidities, such as arrhythmias, chronic liver disease, protein-losing enteropathy, thromboembolic issues, heart failure, dysfunction of the ventricles and valves, renal failure, and plastic bronchitis.
Q: What exactly is Glenn shunt?
A: During the Glenn surgery, the surgical team detaches the superior vena cava (SVC) from the heart and connects it to the pulmonary artery. As a result of this procedure, blood from the upper body is rerouted to flow directly into the pulmonary artery, which is responsible for conveying blood to the lungs.
