Best PDA Device Closure Cost in India
- The cost of PDA Closure Surgery in India ranges between USD 4200 to USD 5000.
- The success rate of PDA surgery is 95%. In some cases risks like infection, headache, fever or allergic reaction to the nickel component of the device may occur.
- A patient needs to spend approximately 4 days in the hospital and 7 days outside of the hospital.
- Tests like Echocardiography, Chest X-Ray, ECG and Doppler study are required to diagnose PDA.
What is PDA?
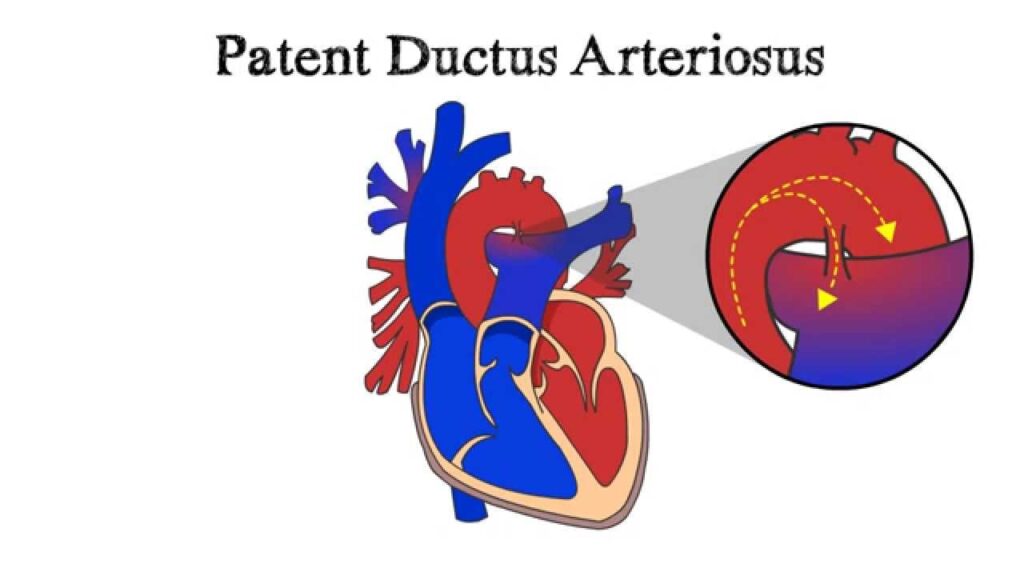
Patent ductus arteriosus (PDA) is a heart problem that occurs soon after birth in some babies. In PDA, abnormal blood flow occurs between two of the major arteries connected to the heart.
Before birth, the two major arteries-the aorta and the pulmonary (PULL-mun-ary) artery-are connected by a blood vessel called the ductus arteriosus. This vessel is an essential part of fetal blood circulation.
Within minutes or up to a few days after birth, the vessel is supposed to close as part of the normal changes occurring in the baby’s circulation.
In some babies, however, the ductus arteriosus remains open (patent). This opening allows oxygen-rich blood from the aorta to mix with oxygen-poor blood from the pulmonary artery. This can put strain on the heart and increase blood pressure in the lung arteries.
Overview
A PDA is a type of congenital heart defect. A congenital heart defect is any type of heart problem that’s present at birth.
If your baby has a PDA but an otherwise normal heart, the PDA may shrink and go away. Some children need treatment to close their PDAs.
If your baby is born with another heart defect (in addition to PDA) that decreases blood flow from the heart to the lungs or that decreases the flow of oxygen-rich blood to the body, medicine may be given to keep the ductus arteriosus open.
This helps maintain blood flow and oxygen levels until doctors can do corrective surgery for the heart defect.
Symptoms
Patent ductus arteriosus symptoms vary with the size of the defect and whether the baby is full term or premature. A small PDA might cause no signs or symptoms and go undetected for some time — even until adulthood. A large PDA can cause signs of heart failure soon after birth.
Your baby’s doctor might first suspect a heart defect during a regular checkup after hearing a heart murmur while listening to your baby’s heart through a stethoscope.
A large PDA found during infancy or childhood might cause:
- Poor eating, which leads to poor growth
- Sweating with crying or eating
- Persistent fast breathing or breathlessness
- Easy tiring
- Rapid heart rate.
Causes
Congenital heart defects arise from problems early in the heart’s development — but there’s often no clear cause. Genetic factors might play a role.
Before birth, an opening that connects two major blood vessels leading from the heart — the aorta and pulmonary artery — is necessary for a baby’s blood circulation. The connection diverts blood from a baby’s lungs while they develop, and the baby receives oxygen from the mother’s circulation.
After birth, the ductus arteriosus normally closes within two or three days. In premature infants, the opening often takes longer to close. If the connection remains open, it’s referred to as a patent ductus arteriosus.
The abnormal opening causes too much blood to flow to the baby’s lungs and heart. Untreated, the blood pressure in the baby’s lungs might increase (pulmonary hypertension) and the baby’s heart might enlarge and weaken.
Risk factors
Risk factors for having a patent ductus arteriosus include:
1. Premature birth. A patent ductus arteriosus occurs more commonly in babies who are born too early than in babies who are born full term.
2. Family history and other genetic conditions. A family history of heart defects and other genetic conditions, such as Down syndrome, increase the risk of having a PDA.
3. Rubella infection during pregnancy. If you contract German measles (rubella) during pregnancy, your baby’s risk of heart defects increases. The rubella virus crosses the placenta and spreads through the baby’s circulatory system, damaging blood vessels and organs, including the heart.
4. Being born at a high altitude. Babies born above 8,200 feet (2,499 meters) have a greater risk of a PDA than babies born at lower altitudes.
5. Being female. PDA is twice as common in girls.
PDA Device Closure Complications?
A small patent ductus arteriosus might not cause complications. Larger, untreated defects could cause:
High blood pressure in the lungs. Too much blood circulating through the heart’s main arteries through a patent ductus arteriosus can lead to pulmonary hypertension, which can cause permanent lung damage. A large patent ductus arteriosus can lead to Eisenmenger syndrome, an irreversible type of pulmonary hypertension.
Heart failure. A patent ductus arteriosus can eventually cause the heart to enlarge and weaken, leading to heart failure, a chronic condition in which the heart can’t pump effectively.
Heart infection (endocarditis). People who have structural heart problems, such as a patent ductus arteriosus, are at a higher risk of an inflammation of the heart’s inner lining than are people who have healthy hearts.
Diagnosis
The doctor might suspect that you or your child has a patent ductus arteriosus based on you or your child’s heartbeat. A PDA can cause a heart murmur that the doctor can hear through a stethoscope.
If the doctor suspects a heart defect, he or she might request one or more of the following tests:
- Echocardiogram. Sound waves produce images of the heart that can help the doctor identify a PDA, see if the heart chambers are enlarged, and judge how well the heart is pumping. This test also helps the doctor evaluate the heart valves and detect other potential heart defects.
- Chest X-ray. An X-ray image helps the doctor see the condition of your or your baby’s heart and lungs. An X-ray might reveal conditions other than a heart defect, as well.
- Electrocardiogram. This test records the electrical activity of the heart, which can help the doctor diagnose heart defects or rhythm problems.
- Cardiac catheterization. This test isn’t usually necessary for diagnosing a PDA alone, but it might be done to examine other congenital heart defects found during an echocardiogram or if a catheter procedure is being considered to treat a PDA.
A thin, flexible tube (catheter) is inserted into a blood vessel at your or your child’s groin or arm and guided through it into the heart. Through catheterization, the doctor may be able to do procedures to close the patent ductus arteriosus.
Types of Treatment
Treatments for a patent ductus arteriosus depend on the age of the person being treated. Options might include:
- Watchful waiting. In a premature baby, a PDA often closes on its own. The doctor will monitor your baby’s heart to make sure the open blood vessel is closing properly. For full-term babies, children and adults who have small PDAs that aren’t causing other health problems, monitoring might be all that’s needed.
- Medications. In a premature baby, nonsteroidal anti-inflammatory drugs (NSAIDs) — such as ibuprofen (Infants’ Advil, Infants’ Motrin, others), available over the counter, or indomethacin (Indocin), available by prescription — might be used to help close a PDA. NSAIDs block the hormonelike chemicals in the body that keep the PDA open. NSAIDs won’t close a PDA in full-term babies, children or adults.
- Surgical closure. If medications aren’t effective and your child’s condition is severe or causing complications, surgery might be recommended. A surgeon makes a small cut between your child’s ribs to reach your child’s heart and repair the open duct using stitches or clips.
After the surgery, your child will remain in the hospital for several days for observation. It usually takes a few weeks for a child to fully recover from heart surgery. Occasionally, surgical closure might also be recommended for adults who have a PDA that’s causing health problems. Possible risks of the surgery include hoarseness, bleeding, infection and a paralyzed diaphragm.
- Catheter procedures. Premature babies are too small for catheter procedures. However, if your baby doesn’t have PDA-related health problems, the doctor might recommend waiting until the baby is older to do a catheter procedure to correct the PDA. Catheter procedures can also be used to treat full-term babies, children and adults.
In a catheter procedure, a thin tube (catheter) is inserted into a blood vessel in the groin and threaded up to the heart. Through the catheter, a plug or coil is inserted to close the ductus arteriosus.
If the procedure is done on an outpatient basis, you or your child probably won’t stay overnight in the hospital. Complications from catheter procedures include bleeding, infection, or movement of the plug or coil from where it was placed in the heart.
Before Procedure
Medical history noted and clinical examination of the child performed
Adviced general tests to check for fitness of surgery
Counselled regarding the procedure
PDA Closure Procedure
- Procedure usually takes about 1 to 3 hours.
- Usually performed in cardiac catherization lab.
- Access in the femoral vein is obtained with placement of a sheath. A sheath is placed in the femoral artery.
The device is then advanced to the tip of the sheath in the descending aorta The sheath and device are then pulled back into a position. - When good position is achieved, the sheath is retracted further and the tubular part of the device is opened within the PDA.
- Angiogram is performed in the descending aorta to confirm final device position up to this step, the device can be repositioned or retrieved if the angiogram showed significant residual flow.
- Occasionally a repeat angiogram is performed in the descending aorta ten minutes after.
- If device position is satisfactory, the device is released.
After Procedure
1. The patient is hospitalized for a day to monitor the vitals.
2. An X-ray and echo doppler study performed the next day after the procedure to make sure the closure device has not moved.
3. Usually discharged after evaluationand kept on oral antibiotic.
4. Subacute bacterial endocarditis prophylaxis is recommended for six months or until complete closure is obtained.
5. Cardiologist may advise some physical activity restrictions for a short time.
6. Pregnancy is low risk in patients with PDA unless there is pulmonary hypertension or signs of heart failure.
7. Follow-up the patient includes clinical evaluation, transthoracic echocardiography and CXR done at regular intervals.
Precautions after pda closure
There’s no sure way to prevent having a baby with a patent ductus arteriosus. However, it’s important to do everything possible to have a healthy pregnancy. Here are some of the basics:
- Seek early prenatal care, even before you’re pregnant. Quitting smoking, reducing stress, stopping birth control — these are all things to talk to your doctor about before you get pregnant. Also discuss medications you’re taking.
- Eat a healthy diet. Include a vitamin supplement that contains folic acid.
- Exercise regularly. Work with your doctor to develop an exercise plan that’s right for you.
- Avoid risks. These include harmful substances such as alcohol, cigarettes and illegal drugs. Also avoid hot tubs and saunas.
- Avoid infections. Update your vaccinations before becoming pregnant. Certain types of infections can be harmful to a developing baby.
- Keep diabetes under control. If you have diabetes, work with your doctor to manage the condition before and during pregnancy.
- If you have a family history of heart defects or other genetic disorders, consider talking with a genetic counselor before becoming pregnant.
Frequently Asked Questions About PDA Device Closure
Q. What Is Patent Ductus Arteriosus?
A. Patent ductus arteriosus (PDA) is an extra blood vessel found in babies before birth and just after birth.
Q. When is PDA first suspected in infants?
A. In full-term infants, patent ductus arteriosus (PDA) usually is first suspected when the baby’s doctor hears a heart murmur during a regular checkup.
A heart murmur is an extra or unusual sound heard during the heartbeat. Heart murmurs also have other causes besides PDA, and most murmurs are harmless.
Q: Why is the size of PDA important in planning treatment?
A small PDA frequently does not cause problems and might never necessitate treatment. But, a larger PDA, if left untreated, can lead to poorly oxygenated blood flow in the wrong direction, failing the heart muscle and leading to heart failure accompanied by other complications.
Q. Who will treat children with PDA?
A: A pediatric cardiologist is qualified in treating the condition in children.
Q. Can PDA close on its own?
A. In most babies who have an otherwise normal heart, the PDA will shrink and close on its own in the first few days of life. If it stays open longer, it may cause extra blood to flow to the lungs



