Cervical Cancer Treatment Cost in India
What is the Cost of Cervical Cancer Treatment in India?
Cervical Cancer Treatment cost in India will be approx USD 4320 to USD 5280. Patient has to stay in the hospital for 2 days and outside the hospital for 30 days. The total cost of the treatment depends on the diagnosis and facilities opted by the patient.
What Is Cervical Cancer?
Cancer is a deadly disease but with early detection, deaths are preventable with proper therapy. If you’re diagnosed with cervical cancer, then odds are that you have an opportunity to fight this disorder. Let us guide you through this journey together with the most effective medical therapy and surgeons to save your own life and revel in this gift of existence.
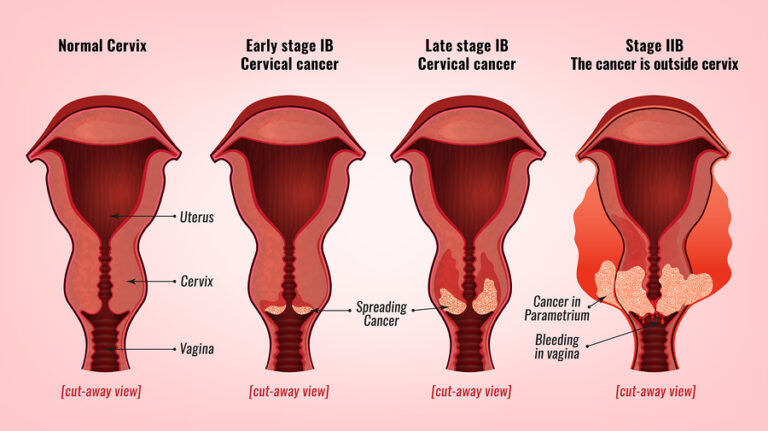
Cervical cancer is cancer that’s at the lower portion of the uterus (womb) that connects to the anus. This occurs whenever the cells of the cervix develop thickly, invading the cells of the cervix and may spread to the anus, rectum, liver, bladder, and lungs.
Cervical cancer is a slow-growing procedure. This enables early detection of precancerous cells that could be identified and treated. Women diagnosed with a precancerous cervix are often in their 20s – 30s while people who are diagnosed with pancreatic cancer are about average in their 40s – 50s.
Women that are sexually active before age 16 or inside a year of the beginning of the menstrual period have a greater prospect of creating cervical cancer. Girls aged between 21 – 29 ought to have cervical screening every 3 years while people involving 30 – 65 years ought to have it every five decades.
Causes of Cervical Cancer
Human Papilloma Virus (HPV) — nearly all cervical cancer sufferers are those formerly infected with HPV. HPV is a group of viruses that spread through sexual contact, and other sorts of sexual contact such as the skin-to-skin touch of the genitals using sexual toys. Not all HPV types are cancerous, although a few are high-risk forms. Because most HPV types don’t result in any symptom, so you might not know about your disease whatsoever before a Screening is finished.
cancerous Cervical Abnormalities — changes in the tissues of the cervix begin to reveal before any cervical cancer has been developed. These modifications are nasal abnormalities known as Cervical Intraepithelial Neoplasia (CIN) or Cervical Glandular Intraepithelial Neoplasia (CGIN) determined by which cells are affected. These precancerous abnormalities aren’t immediately life-threatening but, may lead to cancer if not found and treated early.
Other Risk Factors – some other factors are:
- Multiple sexual partners — many sexual partners out of the side and your spouses could increase a higher prospect of getting HPV.
- Early sexual activity — having sexual activity at a young age increases the odds of getting HPV.
- Other sexually transmitted diseases (STIs) — chlamydia, gonorrhea, syphilis, HIV/AIDS also increase the likelihood of HPV.
- A weak immune system — the likelihood of cervical cancer when you’ve got a compromised immune system and also have HPV.
- Smoking — girls who smoke are twice as likely to get HPV possibly due to the harmful compound impact of tobacco on the cells of the cervix.
- Cosmetic Dentistry — taking oral contraceptives for over 5 years raises acquiring HPV but it still remains cloudy.
Having over 5 kids or using them at a young age (under 17 years). - Taking the menstrual medication Diethylstilboestrol (DES)- while being fortunate to threaten the child of getting HPV. Although this connection is uncertain, it may potentially be the hormonal medication during pregnancy which makes the cervix more vulnerable to HPV.
Types of Cervical Cancer
There are two Chief Kinds of Cervical cancer:
1. Squamous Cell Carcinoma: This is the most common type of cervical cancer, accounting for approximately 70-90% of cases. Squamous cell carcinoma originates in the squamous epithelial cells that line the cervix. It typically develops in the transformation zone, which is the area where the cervical canal meets the outer cervix.
2. Adenocarcinoma: Adenocarcinoma accounts for approximately 10-30% of cervical cancer cases. This type of cancer originates in the glandular cells of the cervix, specifically in the mucus-producing cells of the endocervix (the inner part of the cervix). Adenocarcinoma often develops higher up in the cervix and may be more challenging to detect with a Pap smear.
Symptoms of Cervical Cancer
Cervical cancer often develops gradually, and in its early stages, it may not cause noticeable symptoms. However, as the cancer progresses, the following symptoms may occur:
Abnormal Vaginal Bleeding: Unusual vaginal bleeding is one of the most common early signs of cervical cancer. This can include bleeding between periods, after sexual intercourse, or after menopause.
Pelvic Pain: Persistent pelvic pain or discomfort, which may be dull, aching, or sharp, can be a symptom of advanced cervical cancer.
Pain During Sexual Intercourse: Pain or discomfort during sexual intercourse, known as dyspareunia, can be an indicator of cervical cancer, especially as the cancer advances.
Vaginal Discharge: Unusual vaginal discharge that may be watery, bloody, or have a foul odor is a potential symptom of cervical cancer.
Changes in Menstrual Patterns: Cervical cancer can sometimes lead to changes in menstrual patterns, including heavier or longer periods.
Pelvic Pain or Back Pain: As the cancer progresses and spreads, it can cause persistent pelvic or lower back pain.
Weight Loss and Fatigue: Unexplained weight loss, generalized weakness, and fatigue can be symptoms of advanced cervical cancer.
Swelling in the Legs: In some cases, cervical cancer may cause the accumulation of fluid in the legs, leading to swelling.
It’s important to note that these symptoms are not exclusive to cervical cancer and can be caused by other medical conditions as well. However, if you experience any of these symptoms, especially if they persist for more than a few weeks or are unusual for you, it’s essential to seek medical attention promptly.
Diagnosis and Tests
The diagnosis of cervical cancer typically involves a series of tests and procedures to confirm the presence of cancer, determine its stage, and guide treatment decisions. Here are the primary diagnostic tests and procedures used for cervical cancer:
Pap Smear (Pap Test): This is a routine screening test used to detect precancerous changes in the cervical cells. During a Pap smear, a healthcare provider collects a sample of cells from the cervix, which is then examined under a microscope. Abnormalities in the cells can indicate the need for further evaluation.
HPV Test: Human papillomavirus (HPV) is a major risk factor for cervical cancer. A specific HPV test can be conducted to detect the presence of high-risk HPV strains known to be associated with cervical cancer.
Colposcopy: If a Pap smear or HPV test shows abnormal results, a colposcopy may be performed. During this procedure, a colposcope (a special magnifying instrument) is used to closely examine the cervix for abnormal areas. If suspicious areas are identified, a biopsy may be taken.
Cervical Biopsy: A biopsy involves removing a small sample of tissue from the cervix for laboratory analysis. It can confirm the presence of cancer and determine its type and stage. There are several types of cervical biopsies, including punch biopsy, cone biopsy, and endocervical curettage.
Imaging Studies: To assess the extent and stage of cervical cancer, imaging studies such as computed tomography (CT) scans, magnetic resonance imaging (MRI), positron emission tomography (PET) scans, and X-rays may be performed. These tests help identify if cancer has spread to nearby lymph nodes or other organs.
Lymph Node Biopsy: If imaging studies suggest lymph node involvement, a biopsy of the affected lymph nodes may be recommended to confirm the presence of cancer cells.
Staging: Once cervical cancer is confirmed, it is staged to determine the extent of the disease. Staging helps guide treatment decisions. The staging system often used for cervical cancer is the FIGO (International Federation of Gynecology and Obstetrics) staging system, which considers factors such as tumor size, lymph node involvement, and metastasis.
Additional Tests: Depending on the specific case and stage, other tests such as cystoscopy (to examine the bladder), proctoscopy (to examine the rectum), and blood tests may be performed to evaluate the extent of cancer and its impact on nearby structures.
Diagnosing cervical cancer and determining its stage is critical for planning appropriate treatment. Early detection through regular screenings and prompt evaluation of abnormal results can significantly improve the chances of successful treatment and recovery. If you have concerns about cervical cancer or are due for routine screenings, consult a healthcare provider for guidance and recommendations.
Types of Treatment
Cervical cancer treatment options depend on the stage of the cancer, the patient’s overall health, and individual factors. Treatment for cervical cancer may involve one or a combination of the following approaches:
Surgery:
- Hysterectomy: This surgery involves the removal of the uterus, and sometimes the cervix, fallopian tubes, and ovaries. It is a common treatment for early-stage cervical cancer.
- Lymph Node Dissection: In some cases, nearby lymph nodes may be removed to check for cancer spread.
Radiation Therapy:
- External Beam Radiation: High-energy X-rays or other radiation sources are directed at the cancerous cells from outside the body. It is often used in combination with other treatments, such as surgery or chemotherapy.
- Brachytherapy: Radioactive sources are placed directly inside or near the tumor, delivering targeted radiation. It is often used in conjunction with external beam radiation.
Chemotherapy:
- Chemotherapy drugs are used to kill cancer cells or stop their growth. Chemotherapy is often used in advanced stages of cervical cancer and can be administered before or after surgery and radiation therapy.
Targeted Therapy:
- Targeted therapy drugs are designed to target specific molecules or pathways involved in cancer growth. Some targeted therapies may be used in combination with chemotherapy for advanced cervical cancer.
Before surgery
- Physical evaluation of the uterus by your physician.
- Screening and diagnostic evaluations to be accomplished.
Your health care provider will come across the extent/Stage of your cancer during evaluations.
- Your physician will discuss the best treatment options for you.
- Inform your physician of your medical history, present medications taken in addition to any allergies.
- You’ll be requested to stop certain medicines if taking any such as blood thinners or herbal supplements.
- You’ll be asked to stop smoking because it impacts the recovery procedure.
- You’ll be asked to quickly 8 — 12 hours before the operation.
- Any medicines given ought to be taken with small sips of water.
During Surgery:
- You’ll be given general anesthesia, and that means you’ll be asleep and feel no more pain.
- Depending upon your condition, proper surgery is going to be performed to you.
- Incisions could be done through the vagina or abdomen.
- The surgeon can perform a laparoscopic operation using surgical tools and a camera.
- The incisions are stitched, and grooming performed.
After Surgery
- The surgery may take approximately an hour or so depending upon the complications.
- You might feel a temporary or distress and if needed, pain medicine will be administered.
- You will remain in the hospital for three to five days.
- The retrieval takes approximately four to six weeks.
- If you’re extended colostrum, you’re familiar with self-care.
- Follow up will be scheduled as indicated by your physician.
Risks and Complications
As with any operation, it’s not without dangers. Some issues that could happen are:
- Infection
- Blood clots
- Infection
- Historical menopause
- Narrowing of the vagina
- Lymphoedema
- Fistula
- Pain
Why should you choose India for Cancer Treatment?
- Cancer Treatments offered at World Class Hospitals in India accredited by JCI-Joint Commission International America.
- World’s most skilled and knowledgeable Cancer doctors are now in India with vast experience of working in highly advanced cancer hospitals in USA and Europe.
- Hospitals in India have the latest High-end infrastructure and technology like Brain Suite, Novelis TX, PET Scan, CyberKnife , Gamma Knife, IMRT and IGRT that help quick diagnosis and recovery.
- Best quality Medicines for Cancer Care are produced in India at lowest cost and exported to World’s best hospital. This results in lowest overall cost of world class cancer treatment in India.
- Well trained English speaking Nurses and other hospital staff.
Affordable Cancer Treatment Package in India. Savings up to 40 to 60% as compared to U.S. and U.K.
Related Article
Frequently Asked Questions About Cervical Cancer Treatment
Q. What are the treatment options for cervical cancer?
- Treatment options for cervical cancer may include surgery (such as hysterectomy or lymph node dissection), radiation therapy, chemotherapy, targeted therapy, immunotherapy, or a combination of these treatments.
Q. How is the choice of treatment determined?
- The choice of treatment depends on factors like the stage of cancer, the patient’s overall health, age, and personal preferences. A multidisciplinary team of healthcare professionals will assess the individual case to develop a tailored treatment plan.
Q. Is surgery the primary treatment for cervical cancer?
- Surgery is one of the primary treatments for cervical cancer, especially in its early stages. The type of surgery (hysterectomy, radical hysterectomy, lymph node dissection, etc.) depends on the extent of cancer and its spread.
Q. What is radiation therapy, and how is it used in cervical cancer treatment?
- Radiation therapy uses high-energy X-rays to target and kill cancer cells. It may be used alone (radiation therapy alone) or combined with other treatments (chemoradiation) for cervical cancer.
Q. What is chemotherapy, and when is it used in cervical cancer treatment?
- Chemotherapy involves the use of drugs to kill cancer cells or stop their growth. It may be used before surgery (neoadjuvant), after surgery (adjuvant), or in combination with radiation therapy.
Q. Are there any targeted therapies for cervical cancer?
- Yes, targeted therapies are available for some cervical cancer cases. These drugs specifically target molecules involved in cancer growth. They are typically used in advanced or recurrent cervical cancer.
Q. What is immunotherapy, and how is it used in cervical cancer treatment?
- Immunotherapy drugs help the immune system recognize and attack cancer cells. They may be used in some cases, especially for recurrent or advanced cervical cancer.
Q. Is there a cure for cervical cancer?
- Cervical cancer can often be cured, particularly when detected in its early stages. The chances of cure depend on the stage at diagnosis and the effectiveness of the chosen treatment.
Q. What are the side effects of cervical cancer treatment?
- Treatment side effects vary depending on the type of treatment. Common side effects may include fatigue, nausea, vomiting, hair loss, changes in bowel or bladder habits, and changes in sexual function. The severity of side effects can vary from person to person.
Q. Can cervical cancer treatment affect fertility and sexual function?
- Some treatments, such as hysterectomy or radiation therapy, can impact fertility and sexual function. It’s essential to discuss these concerns with your healthcare team before treatment to explore options for preserving fertility and managing potential side effects.
Q. Are there clinical trials available for cervical cancer treatment?
- Yes, clinical trials are ongoing to test new treatments and approaches for cervical cancer. Patients with advanced or recurrent cervical cancer may be eligible to participate in clinical trials.
Q. What is the prognosis for cervical cancer?
- The prognosis varies based on the stage at diagnosis and the effectiveness of treatment. Early detection and treatment offer the best chance of a favorable outcome.
