Hysterectomy Surgery Cost in India
The average cost of Hysterectomy Surgery in India is approximately USD 2000 to USD 5000. However, the prices may vary depending upon the hospitals in different cities.
Overview
Hysterectomy involves the surgical removal of the uterus. This procedure is performed to address conditions such as cancer, irregular bleeding, fibroids, and uterine prolapse. There are several reasons why women might require a hysterectomy. The surgery is done to treat a variety of chronic pain issues, as well as certain forms of cancer and infections. Depending on the condition, the doctor will suggest whether a patient needs an abdominal, vaginal, or laparoscopic hysterectomy.
Usually, the time required for an abdominal and vaginal hysterectomy is between 60 to 90 minutes, while a laparoscopic hysterectomy takes around 120 minutes. A hysterectomy is considered a very safe treatment, although patients may need to spend at least a day in the hospital afterwards. However, they might be asked to stay for a few more days if required.
Although it’s considered safe, there are certain risks and complications associated with the surgery. Some of the common complications of hysterectomy are infections, vaginal bleeding, harm to surrounding organs, and other risks frequently connected with hysterectomies. After the surgery, individuals typically require sanitary pads due to significant bleeding and vaginal discharge. Even after the surgery, there might be a possibility of experiencing vaginal discharge for a few weeks. This is considered typical and not a cause for alarm.
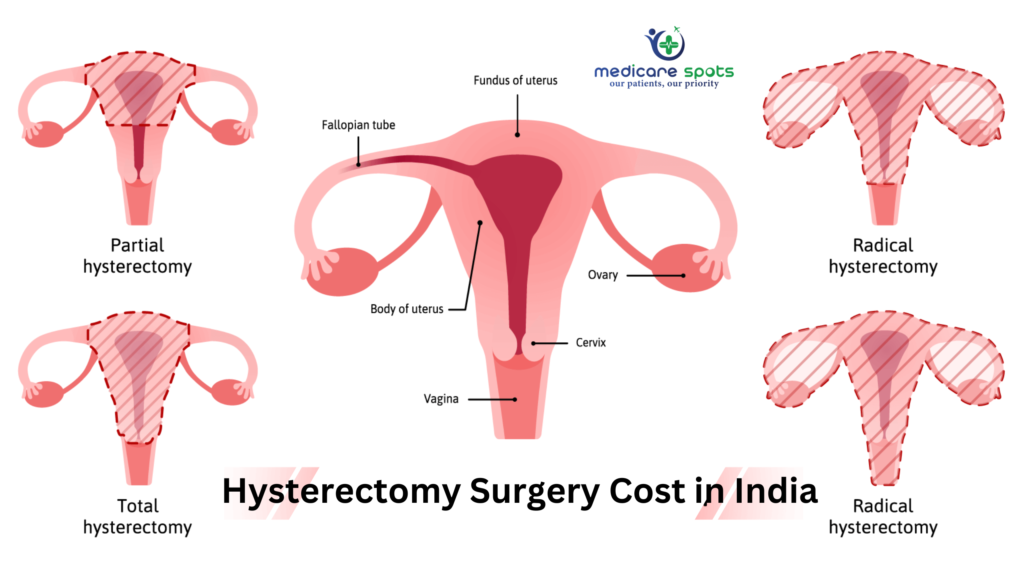
Types of Hysterectomy
There are three types of hysterectomy. The doctor would suggest which hysterectomy procedure patients require, depending on the seriousness or complexity of the condition:
Radical Hysterectomy: Radical hysterectomy is usually done to remove the uterus, the cervix, the upper vaginal wall, and supporting tissues. It may also be recommended in cases of cancer. Bilateral salpingo-oophorectomy is the medical term for a radical hysterectomy in which both ovaries and both fallopian tubes are removed. This might cause induced or medical menopause after the removal of the ovaries before a woman reaches natural menopause.
Partial or Subtotal Hysterectomy: The cervix is left intact, and the upper two-thirds of the uterus are removed during a partial hysterectomy. This is best for women who have never had an abnormal Pap smear test. The patient will need to continue monitoring for cervical cancer with regular pap smear tests. Also, partial hysterectomy can be carried out abdominally or laparoscopically.
Complete or Total Hysterectomy: The uterus and cervix are both removed during total hysterectomy. A total hysterectomy reduces the likelihood of future cervical or endometrial cancer.
Hysterectomy has been a highly effective surgery for women with adverse gynaecological complications, as it provides immediate and permanent relief.
The type of hysterectomy performed determines the length of recovery and healing after surgery. Patients must strictly follow all the doctor’s guidelines to hasten the healing process. After surgery, it is best to refrain from strenuous exercise and heavy lifting after surgery. For a few weeks, it is recommended to avoid sexual activity until the scars are healed and the vaginal discharge ceases. Walking is the most advised kind of exercise after surgery because it helps strengthen pelvic and lower body muscles.
Diagnosis for Hysterectomy
Hysterectomy impacts a woman’s hormonal balance and overall health for a lifetime. Because of this, surgery is usually resorted to just as the last treatment, when other therapies are ineffective, to deal with specific conditions for example:
Uterine fibroids: Benign lumps that grow in the uterus resulting in abnormal menstrual bleeding, prostate issues, difficult bowel movements, infertility, and other pregnancy issues.
Endometriosis: A layering of tissue outside the uterus, this also causes significant periods, infertility, and abdominal discomfort.
Chronic pelvic pain: Pain that happens under the belly button and also in between the hips which lasts more than six months. The causes are diverse and may result from endometriosis, musculoskeletal problems, irritable gut syndrome, cystitis, urinary tract disease, fibroids and several other instances.
Adenomyosis: Similar to Infection, this happens when the muscle tissue of the uterus is inhabited from the cells that line the uterus. The symptoms include heavy periods, spotting during periods, painful periods, periods lasting more than normal and, feeling of pressure in the rectum or bladder.
Uterine prolapse: once the muscles or ligaments are no more able to encourage the uterus due to extending or weakening of the muscles, it induces prolapse where the uterus slips from the place into the anus, outside the vagina or birth canal. This induces vaginal bleeding, difficulties with sexual intercourse, higher release, recurrent kidney infections, constipation, and distress in the pelvis.
Placenta praevia or placenta percreta: whenever there’s a serious case of the placenta positioning itself close or within the cervical opening or, attaches itself unnaturally into the esophageal wall. It’s done postpartum and requires vaginal bleeding during pregnancy with or without the pain.
Cancer of the uterus, cervix or ovaries: takes place when cancerous, abnormal development of cells is observed in these regions causing vaginal bleeding, pelvic pain, abnormal discharge, pain during sexual activity, urinary troubles, etc.
What happens during a hysterectomy?
Your healthcare provider will determine the type of hysterectomy you need and the best surgical method to perform that procedure. You’ll change into a hospital gown and get hooked up to monitors that track your heart rate. An intravenous (IV) line is placed in a vein in your arm to deliver medications and fluids.
An anesthesiologist will give you either:
- General anesthesia, in which you won’t be awake during the procedure; or
- Regional anesthesia (also called epidural or spinal anesthesia), in which medications are placed near the nerves in your lower back to “block” pain while you stay awake.
- There are several different surgical approaches your healthcare provider may use to perform a hysterectomy:
Vaginal hysterectomy
- Your uterus is removed through an incision at the top of your vagina. There isn’t an external incision.
- Dissolvable stitches are placed inside your vagina.
- Most commonly used in cases of uterine prolapse and other nonmalignant (or noncancerous) conditions.
- Fewest complications and fastest recovery (up to four weeks) and considered the preferred approach.
- People often go home on the same day of surgery.
Laparoscopic hysterectomy
- A laparoscope (a thin tube with a video camera on the end) is inserted in your lower abdomen through a small incision in your belly button.
- Surgical tools are inserted through several other small incisions.
- Your uterus can be removed in small pieces through the incisions in your abdomen or through your vagina.
- Some people go home the same day or after one night in the hospital.
- Full recovery is shorter and less painful than an abdominal hysterectomy.
Robotic-assisted laparoscopic hysterectomy
- Your surgeon performs the procedure with the help of a robotic machine.
- A laparoscope is inserted in your abdomen so your pelvic area can be viewed.
- Small, thin surgical tools are inserted through three to five incisions around your belly button. Robotic arms and instruments are controlled by the surgeon.
- The recovery is similar to a laparoscopic hysterectomy.
Abdominal hysterectomy
- Your uterus is removed through a six- to eight-inch-long incision in your abdomen.
- The incision is made either from your belly button to your pubic bone or across the top of your public hairline. The surgeon will use stitches or staples to close the incision.
- Most commonly used when cancer is involved, when the uterus is enlarged or when disease spreads to other pelvic areas.
- It generally requires a longer hospital stay (two or three days) and a longer recovery time.
What are the complications of a hysterectomy?
As with any surgery, there’s a slight chance that problems may occur, including:
- Blood clots.
- Severe infection.
- Bleeding.
- Bowel blockage.
- Torn internal stitches.
- Urinary tract injury.
- Issues related to anesthesia.
Related Articles
Frequently asked questions (FAQs) about hysterectomy?
Q. What is a hysterectomy?
A. A hysterectomy is a surgical procedure in which a woman’s uterus is removed. In some cases, it may also involve the removal of the cervix, fallopian tubes, and ovaries.
Q. Why is a hysterectomy performed?
A. Hysterectomies are performed for various medical reasons, including the treatment of conditions such as uterine fibroids, endometriosis, abnormal uterine bleeding, uterine prolapse, and gynecologic cancers.
Q. Are there different types of hysterectomy?
A. Yes, there are several types of hysterectomy, including total hysterectomy, partial hysterectomy, radical hysterectomy, and more. The choice of type depends on the specific condition and the patient’s needs.
Q. Is a hysterectomy reversible?
A. Hysterectomy is generally considered permanent and irreversible. Once the uterus (and possibly other reproductive organs) is removed, a woman can no longer conceive or carry a pregnancy.
Q. How is a hysterectomy performed?
A. Hysterectomies can be performed using various surgical techniques, including abdominal, vaginal, laparoscopic, or robotic-assisted approaches. The method chosen depends on the individual case.
Q. What is the recovery time after a hysterectomy?
A. Recovery time can vary depending on the type of hysterectomy and individual factors. Generally, most women can return to light activities within a few weeks, but it may take several months to fully recover.
Q. Will I go through menopause after a hysterectomy?
A. If the ovaries are removed during the hysterectomy (oophorectomy), it can induce menopause. If the ovaries are preserved, menopause may occur naturally at a later age.
Q. Are there alternative treatments to a hysterectomy?
A. In some cases, alternative treatments or less invasive procedures may be considered, such as medication, uterine artery embolization, or endometrial ablation. The choice depends on the specific condition and its severity.
Q. Will a hysterectomy affect sexual function?
A. Hysterectomy can have varying effects on sexual function. Some women report improved sexual function after the procedure, while others may experience changes in libido or physical sensations. It’s essential to discuss these concerns with your healthcare provider.
Q. What are the potential complications of a hysterectomy?
A. Complications can include infection, bleeding, injury to nearby organs, blood clots, urinary or bowel problems, and emotional or psychological effects.
Q. Can I still have children after a hysterectomy?
A. No, a hysterectomy permanently removes the uterus, making pregnancy impossible. If fertility preservation is a concern, discuss options with
